Emory University Hospital things to do, attractions, restaurants, events info and trip planning

Basic Info
Emory University Hospital
1364 Clifton Rd NE, Atlanta, GA 30322
3.8(674)
Open until 12:00 AM
Save
spot
spot
Ratings & Description
Info
attractions: Emory University's Goizueta Business School, Michael C. Carlos Museum, Schwartz Center for Performing Arts, Theater Emory, Dooley Statue, Rutledge Park, Mathematics and Science Center, Emory University, Candler Lake, Campus Dining, restaurants: Clifton Cafe, Highland Bakery, The Depot by Kaldi's Coffee, Coffee Central, Cox Hall, Kaldi's Coffee in the HSRB, Dobbs Common Table, Brasiliana Pizza - Atlanta, Double Zero, Twisted Taco, local businesses: Northington Gina M MD, Emory University School of Medicine, Robert W. Woodruff Library, The Ridge, Asbury cafe, Bread Coffeehouse, Emory Student Center, Music Department of Emory University, Kaldi's School of Medicine, Emory Village
 Learn more insights from Wanderboat AI.
Learn more insights from Wanderboat AI.Phone
(404) 712-2000
Website
emoryhealthcare.org
Open hoursSee all hours
MonOpen 24 hoursOpen
Plan your stay

Pet-friendly Hotels in Decatur
Find a cozy hotel nearby and make it a full experience.

Affordable Hotels in Decatur
Find a cozy hotel nearby and make it a full experience.

The Coolest Hotels You Haven't Heard Of (Yet)
Find a cozy hotel nearby and make it a full experience.

Trending Stays Worth the Hype in Decatur
Find a cozy hotel nearby and make it a full experience.
Reviews
Live events

Candle making in Atlanta
Mon, Jan 26 • 4:00 PM
Atlanta, Georgia, 30312
View details

Olive Oil Tasting and Mocktail Workshop in Atlanta
Sat, Jan 31 • 3:00 PM
Atlanta, Georgia, 30308
View details

Line Dance Tuesdays with Janice
Tue, Jan 27 • 6:30 PM
4518 North Henry Boulevard #suite 109 Stockbridge, GA 30281
View details
Nearby attractions of Emory University Hospital
Emory University's Goizueta Business School
Michael C. Carlos Museum
Schwartz Center for Performing Arts
Theater Emory
Dooley Statue
Rutledge Park
Mathematics and Science Center
Emory University
Candler Lake
Campus Dining

Emory University's Goizueta Business School
4.9
(39)
Open until 12:00 AM
Click for details

Michael C. Carlos Museum
4.8
(485)
Open until 12:00 AM
Click for details
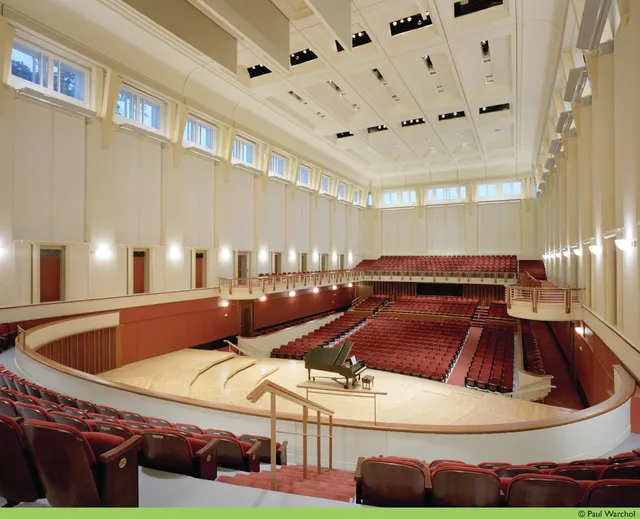
Schwartz Center for Performing Arts
4.9
(42)
Open 24 hours
Click for details

Theater Emory
4.5
(8)
Open until 12:00 AM
Click for details
Nearby restaurants of Emory University Hospital
Clifton Cafe
Highland Bakery
The Depot by Kaldi's Coffee
Coffee Central
Cox Hall
Kaldi's Coffee in the HSRB
Dobbs Common Table
Brasiliana Pizza - Atlanta
Double Zero
Twisted Taco

Clifton Cafe
3.0
(18)
$
Open until 12:00 AM
Click for details

Highland Bakery
3.7
(30)
Click for details

The Depot by Kaldi's Coffee
4.2
(213)
$
Open until 10:00 PM
Click for details

Coffee Central
2.7
(7)
Open until 8:00 PM
Click for details
Nearby local services of Emory University Hospital
Northington Gina M MD
Emory University School of Medicine
Robert W. Woodruff Library
The Ridge
Asbury cafe
Bread Coffeehouse
Emory Student Center
Music Department of Emory University
Kaldi's School of Medicine
Emory Village

Northington Gina M MD
4.3
(5)
Click for details

Emory University School of Medicine
4.6
(7)
Click for details

Robert W. Woodruff Library
4.3
(22)
Click for details

The Ridge
2.4
(22)
Click for details