UH Cleveland Medical Center things to do, attractions, restaurants, events info and trip planning

Basic Info
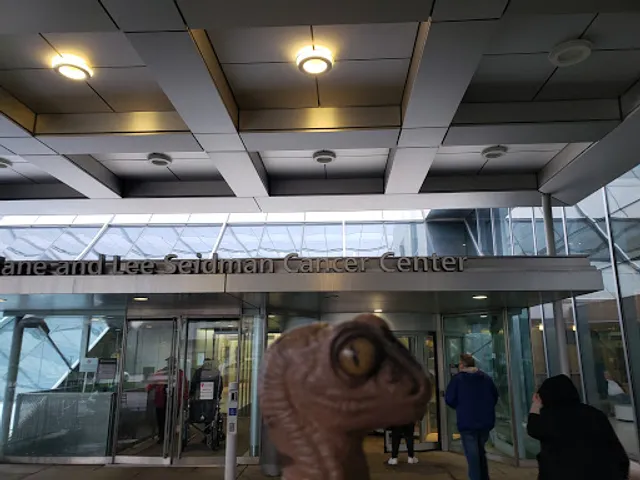
UH Cleveland Medical Center
11100 Euclid Ave, Cleveland, OH 44106
3.1(248)
Open until 12:00 AM
Save
spot
spot
Ratings & Description
Info
attractions: Museum of Contemporary Art Cleveland, Severance Music Center, The Cleveland Orchestra, Case Western Reserve University, The Cleveland Museum of Art, Cozad Bates House, The MOCA Store @ MOCA Cleveland, Cleveland Botanical Garden, One to One Fitness, Tony Brush Park, restaurants: Wolfgang Puck Kitchen Counter, Chopstick Chinese Restaurant, Tacologist Tacos Tequila Margaritas, Rascal House, Hell's Fried Chicken, Kenko Cleveland, Mitchell's Ice Cream (Uptown Shop), The Jolly Scholar, Sittoo's Lebanese Grill University Circle, Sunset Kitchen & Lounge, local businesses: Case Western Reserve University Bookstore, Centric, UH Rainbow Babies & Children’s Hospital, Tinkham Veale University Center, Planet Fitness, Tremont Athletic Club, Dittrick Medical History Center, Cleveland Institute of Art, KakeKutters, Little Italy - University Circle
 Learn more insights from Wanderboat AI.
Learn more insights from Wanderboat AI.Phone
(216) 844-1000
Website
uhhospitals.org
Open hoursSee all hours
WedOpen 24 hoursOpen
Plan your stay

Pet-friendly Hotels in Cleveland
Find a cozy hotel nearby and make it a full experience.

Affordable Hotels in Cleveland
Find a cozy hotel nearby and make it a full experience.

The Coolest Hotels You Haven't Heard Of (Yet)
Find a cozy hotel nearby and make it a full experience.

Trending Stays Worth the Hype in Cleveland
Find a cozy hotel nearby and make it a full experience.
Reviews
Live events

Princess Winter Wonderland at Chick-fil-A North Olmsted
Mon, Feb 2 • 5:30 PM
4779 Great Northern Boulevard North Olmsted, OH 44070
View details

Craft Rock Hall-inspired bracelets
Fri, Jan 30 • 6:00 PM
Cleveland Heights, Ohio, 44118
View details

Cleveland Ghosts Tour
Wed, Jan 28 • 7:00 PM
Brecon, LD3
View details
Nearby attractions of UH Cleveland Medical Center
Museum of Contemporary Art Cleveland
Severance Music Center
The Cleveland Orchestra
Case Western Reserve University
The Cleveland Museum of Art
Cozad Bates House
The MOCA Store @ MOCA Cleveland
Cleveland Botanical Garden
One to One Fitness
Tony Brush Park

Museum of Contemporary Art Cleveland
4.3
(459)
Open until 12:00 AM
Click for details

Severance Music Center
4.9
(1.2K)
Open 24 hours
Click for details

The Cleveland Orchestra
4.8
(244)
Open 24 hours
Click for details

Case Western Reserve University
4.5
(246)
Open 24 hours
Click for details
Nearby restaurants of UH Cleveland Medical Center
Wolfgang Puck Kitchen Counter
Chopstick Chinese Restaurant
Tacologist Tacos Tequila Margaritas
Rascal House
Hell's Fried Chicken
Kenko Cleveland
Mitchell's Ice Cream (Uptown Shop)
The Jolly Scholar
Sittoo's Lebanese Grill University Circle
Sunset Kitchen & Lounge
Wolfgang Puck Kitchen Counter
3.8
(99)
$
Closed
Click for details

Chopstick Chinese Restaurant
3.7
(276)
$
Open until 10:00 PM
Click for details

Tacologist Tacos Tequila Margaritas
4.2
(639)
$
Open until 10:00 PM
Click for details

Rascal House
3.9
(459)
$
Open until 2:30 AM
Click for details
Nearby local services of UH Cleveland Medical Center
Case Western Reserve University Bookstore
Centric
UH Rainbow Babies & Children’s Hospital
Tinkham Veale University Center
Planet Fitness
Tremont Athletic Club
Dittrick Medical History Center
Cleveland Institute of Art
KakeKutters
Little Italy - University Circle

Case Western Reserve University Bookstore
4.1
(184)
Click for details

Centric
4.3
(129)
Click for details

UH Rainbow Babies & Children’s Hospital
3.8
(148)
Click for details

Tinkham Veale University Center
4.6
(228)
Click for details
The hit list

Plan your trip with Wanderboat
Welcome to Wanderboat AI, your AI search for local Eats and Fun, designed to help you explore your city and the world with ease.
Powered by Wanderboat AI trip planner.