Corewell Health William Beaumont University Hospital things to do, attractions, restaurants, events info and trip planning

Basic Info
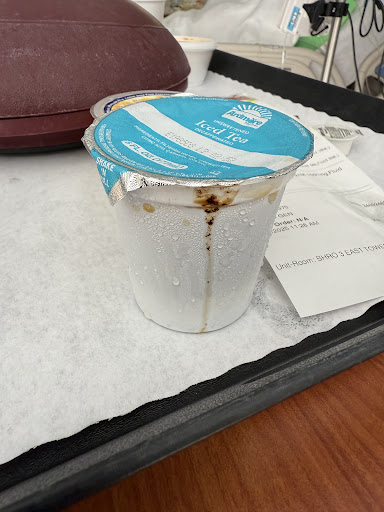
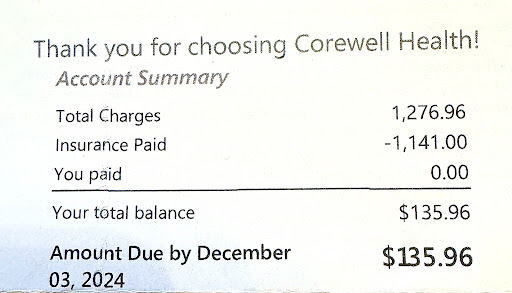
Corewell Health William Beaumont University Hospital
3601 W 13 Mile Rd, Royal Oak, MI 48073
2.7(947)
Open until 12:00 AM
Save
spot
spot
Ratings & Description
Info
attractions: Memorial Park, restaurants: Starbucks Coffee Company, Bucharest Grill, Brown Iron Brewhouse Royal Oak, Nautical Bowls Royal Oak, First Watch, Crumbl, Avenue, Panera Bread, Lucky Detroit Coffee Roasters & Espresso, Super Crab, local businesses: Papa Joe's Royal Oak Beaumont, Woodward Corner Market, Corewell Health William Beaumont University Hospital Laboratory - 3581 W 13 Mile Rd, Woodward Corners by Beaumont, Corewell Health William Beaumont University Hospital Orthopedic Institute - 3535 W 13 Mile Rd, Liquor Supply, Barrels & Vines South, Polestar Detroit, Binson's Medical Equipment and Supplies, Computer Services of Michigan
 Learn more insights from Wanderboat AI.
Learn more insights from Wanderboat AI.Phone
(248) 898-5000
Website
beaumont.org
Open hoursSee all hours
WedOpen 24 hoursOpen
Plan your stay

Pet-friendly Hotels in Royal Oak
Find a cozy hotel nearby and make it a full experience.

Affordable Hotels in Royal Oak
Find a cozy hotel nearby and make it a full experience.

The Coolest Hotels You Haven't Heard Of (Yet)
Find a cozy hotel nearby and make it a full experience.

Trending Stays Worth the Hype in Royal Oak
Find a cozy hotel nearby and make it a full experience.
Reviews
Live events

Create and paint your own pottery
Fri, Jan 30 • 6:00 PM
Grosse Pointe Woods, Michigan, 48236
View details

Essential Detroit tours with Phat Kat
Thu, Jan 29 • 10:00 AM
Detroit, Michigan, 48202
View details

Candlelight: Featuring Vivaldi’s Four Seasons & More
Thu, Jan 29 • 6:30 PM
300 Willits St, Birmingham, MI, US, 48009
View details
Nearby attractions of Corewell Health William Beaumont University Hospital
Memorial Park

Memorial Park
4.5
(307)
Open until 12:00 AM
Click for details
Nearby restaurants of Corewell Health William Beaumont University Hospital
Starbucks Coffee Company
Bucharest Grill
Brown Iron Brewhouse Royal Oak
Nautical Bowls Royal Oak
First Watch
Crumbl
Avenue
Panera Bread
Lucky Detroit Coffee Roasters & Espresso
Super Crab

Starbucks Coffee Company
3.7
(52)
$
Closed
Click for details

Bucharest Grill
3.7
(413)
$
Closed
Click for details

Brown Iron Brewhouse Royal Oak
4.2
(377)
$$
Closed
Click for details

Nautical Bowls Royal Oak
4.8
(87)
$
Closed
Click for details
Nearby local services of Corewell Health William Beaumont University Hospital
Papa Joe's Royal Oak Beaumont
Woodward Corner Market
Corewell Health William Beaumont University Hospital Laboratory - 3581 W 13 Mile Rd
Woodward Corners by Beaumont
Corewell Health William Beaumont University Hospital Orthopedic Institute - 3535 W 13 Mile Rd
Liquor Supply
Barrels & Vines South
Polestar Detroit
Binson's Medical Equipment and Supplies
Computer Services of Michigan

Papa Joe's Royal Oak Beaumont
4.1
(65)
Click for details

Woodward Corner Market
4.5
(508)
Click for details

Corewell Health William Beaumont University Hospital Laboratory - 3581 W 13 Mile Rd
3.7
(28)
Click for details

Woodward Corners by Beaumont
4.5
(585)
Click for details