Kindred Hospital Houston Medical Center things to do, attractions, restaurants, events info and trip planning

Basic Info
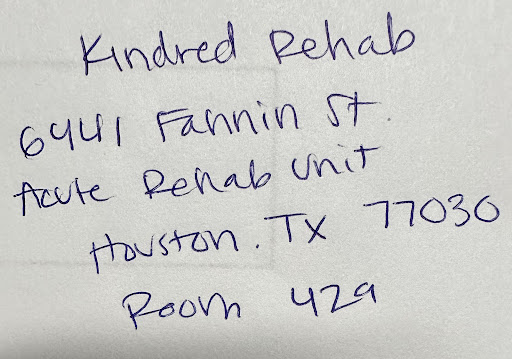
Kindred Hospital Houston Medical Center
6441 Main St, Houston, TX 77030, United States
4.2(207)
Open until 12:00 AM
Save
spot
spot
Ratings & Description
Info
attractions: Palmer Memorial Episcopal Church, Reckling Park, Rice University, DeBakey Library and Museum, Tudor Fieldhouse, James Turrell's "Twilight Epiphany" Skyspace, The Commons, Hermann Park, Hermann Park Playground (The Commons), Buddy Carruth Playground for All Children, restaurants: Miller's Cafe, Alonti Café and Catering Kitchen, Blackwater Coffee Roasters, Piada, Poblano's, South Servery, Memorial Hermann arboretum cafe, The French Corner at Scurlock Tower, Poke In The Bowl, Citadel BBQ, local businesses: 6445 Main St, Houston Methodist Outpatient Center, Memorial Hermann-Texas Medical Center, Children's Memorial Hermann Hospital, UT Physicians Colon & Rectal Clinic - Texas Medical Center, McGovern Medical School at UTHealth Houston, Scurlock Tower, Houston Methodist Hospital, Houston Methodist Hospital - Smith Tower, Yin Yiu, MD
 Learn more insights from Wanderboat AI.
Learn more insights from Wanderboat AI.Phone
+1 713-790-0500
Website
kindredhospitals.com
Open hoursSee all hours
WedOpen 24 hoursOpen
Plan your stay

Pet-friendly Hotels in Houston
Find a cozy hotel nearby and make it a full experience.

Affordable Hotels in Houston
Find a cozy hotel nearby and make it a full experience.

The Coolest Hotels You Haven't Heard Of (Yet)
Find a cozy hotel nearby and make it a full experience.

Trending Stays Worth the Hype in Houston
Find a cozy hotel nearby and make it a full experience.
Reviews
Live events

Hidden Houston Bites: Downtown Food Adventure
Wed, Jan 28 • 11:00 AM
Houston, Texas, 77002
View details

Dining in the Dark: A Unique Blindfolded Dining Experience at Mastrantos
Thu, Jan 29 • 6:00 PM
927 Studewood St 100, Houston, TX, 77008
View details

Custom Candle Making in Houston’s Landmark Shop
Wed, Jan 28 • 11:00 AM
Houston, Texas, 77007
View details
Nearby attractions of Kindred Hospital Houston Medical Center
Palmer Memorial Episcopal Church
Reckling Park
Rice University
DeBakey Library and Museum
Tudor Fieldhouse
James Turrell's "Twilight Epiphany" Skyspace
The Commons
Hermann Park
Hermann Park Playground (The Commons)
Buddy Carruth Playground for All Children

Palmer Memorial Episcopal Church
4.4
(66)
Open 24 hours
Click for details

Reckling Park
4.7
(106)
Open 24 hours
Click for details

Rice University
4.7
(465)
Open 24 hours
Click for details

DeBakey Library and Museum
4.8
(10)
Open until 5:00 PM
Click for details
Nearby restaurants of Kindred Hospital Houston Medical Center
Miller's Cafe
Alonti Café and Catering Kitchen
Blackwater Coffee Roasters
Piada
Poblano's
South Servery
Memorial Hermann arboretum cafe
The French Corner at Scurlock Tower
Poke In The Bowl
Citadel BBQ

Miller's Cafe
4.5
(196)
$
Open until 5:00 PM
Click for details

Alonti Café and Catering Kitchen
4.2
(50)
$$
Click for details

Blackwater Coffee Roasters
4.7
(96)
$
Open until 4:30 PM
Click for details

Piada
4.6
(437)
$
Open until 9:00 PM
Click for details
Nearby local services of Kindred Hospital Houston Medical Center
6445 Main St
Houston Methodist Outpatient Center
Memorial Hermann-Texas Medical Center
Children's Memorial Hermann Hospital
UT Physicians Colon & Rectal Clinic - Texas Medical Center
McGovern Medical School at UTHealth Houston
Scurlock Tower
Houston Methodist Hospital
Houston Methodist Hospital - Smith Tower
Yin Yiu, MD

6445 Main St
4.3
(92)
Click for details

Houston Methodist Outpatient Center
4.3
(60)
Click for details

Memorial Hermann-Texas Medical Center
3.3
(322)
Click for details

Children's Memorial Hermann Hospital
3.3
(236)
Click for details
The hit list

Plan your trip with Wanderboat
Welcome to Wanderboat AI, your AI search for local Eats and Fun, designed to help you explore your city and the world with ease.
Powered by Wanderboat AI trip planner.