Ascension Seton Medical Center Austin things to do, attractions, restaurants, events info and trip planning

Basic Info
Ascension Seton Medical Center Austin
1201 W 38th St, Austin, TX 78705, United States
4.0(977)
Open until 12:00 AM
Save
spot
spot
Ratings & Description
Info
attractions: Seiders Springs Greenbelt, Bailey Neighborhood Park, Shoal Creek Gazebo, Central Park, Ramsey Neighborhood Park, restaurants: Otherside Deli, Santa Rita Cantina, Snooze, an A.M. Eatery, Baretto Bistro, Tiny Boxwoods Austin, 34th Street Café, Mendocino Farms, Kolache Factory, Kerbey Lane Cafe - Central, Tinys Milk & Cookies - Austin, local businesses: Clinical Pathology Laboratories (CPL) - Medical Park Tower, Adelante Boutique, Balm & Bubble: Medspa | Wellness, Benjamin Amis, MD, Clinical Pathology Laboratories (CPL) - Bailey Square, Flower Delivery Austin Same Day Florist, Wood & Rose, Creation Station, Franzetti Jewelers, Bailey Splash Pad
 Learn more insights from Wanderboat AI.
Learn more insights from Wanderboat AI.Phone
+1 512-324-1000
Website
healthcare.ascension.org
Open hoursSee all hours
TueOpen 24 hoursOpen
Plan your stay

Pet-friendly Hotels in Austin
Find a cozy hotel nearby and make it a full experience.

Affordable Hotels in Austin
Find a cozy hotel nearby and make it a full experience.

The Coolest Hotels You Haven't Heard Of (Yet)
Find a cozy hotel nearby and make it a full experience.

Trending Stays Worth the Hype in Austin
Find a cozy hotel nearby and make it a full experience.
Reviews
Live events

Pronto Pilates Arboretum | Grand Opening & Studio Launch Party
Wed, Jan 28 • 5:00 PM
9722 Great Hills Trail #suite 125 Austin, TX 78759
View details

Grand Reopening Celebration
Thu, Jan 29 • 3:00 PM
601 East Whitestone Boulevard ##112 Cedar Park, TX 78613
View details

KidsLinked North Austin – Round Rock Childrens Festival 2026
Fri, Jan 30 • 5:00 PM
3400 East Palm Valley Boulevard Round Rock, TX 78665
View details
Nearby attractions of Ascension Seton Medical Center Austin
Seiders Springs Greenbelt
Bailey Neighborhood Park
Shoal Creek Gazebo
Central Park
Ramsey Neighborhood Park
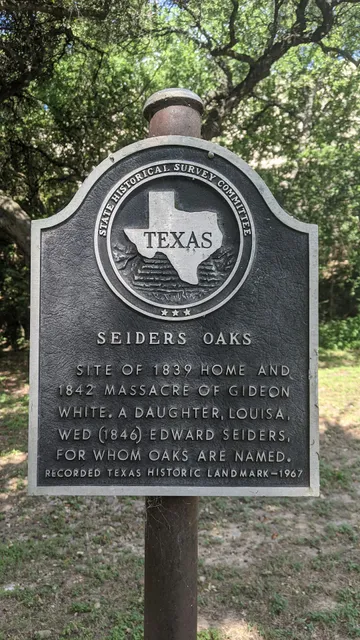
Seiders Springs Greenbelt
4.7
(23)
Closed
Click for details

Bailey Neighborhood Park
4.3
(82)
Closed
Click for details

Shoal Creek Gazebo
3.9
(14)
Open 24 hours
Click for details

Central Park
4.6
(115)
Closed
Click for details
Nearby restaurants of Ascension Seton Medical Center Austin
Otherside Deli
Santa Rita Cantina
Snooze, an A.M. Eatery
Baretto Bistro
Tiny Boxwoods Austin
34th Street Café
Mendocino Farms
Kolache Factory
Kerbey Lane Cafe - Central
Tinys Milk & Cookies - Austin

Otherside Deli
4.8
(276)
$
Closed
Click for details

Santa Rita Cantina
4.0
(431)
$
Closed
Click for details

Snooze, an A.M. Eatery
4.5
(1.6K)
$
Closed
Click for details

Baretto Bistro
4.8
(56)
$$
Closed
Click for details
Nearby local services of Ascension Seton Medical Center Austin
Clinical Pathology Laboratories (CPL) - Medical Park Tower
Adelante Boutique
Balm & Bubble: Medspa | Wellness
Benjamin Amis, MD
Clinical Pathology Laboratories (CPL) - Bailey Square
Flower Delivery Austin Same Day Florist
Wood & Rose
Creation Station
Franzetti Jewelers
Bailey Splash Pad
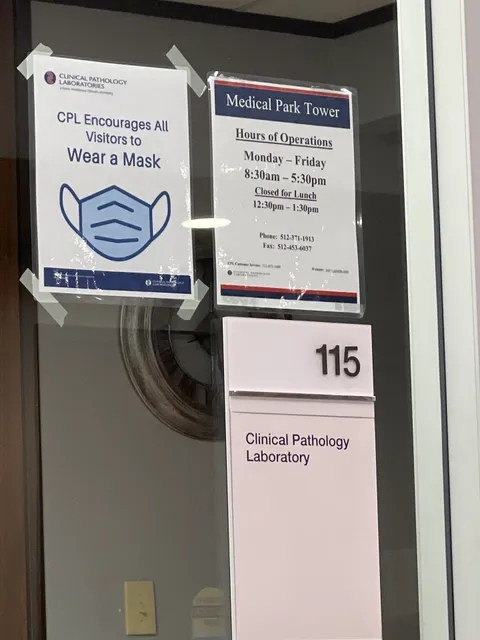
Clinical Pathology Laboratories (CPL) - Medical Park Tower
3.7
(34)
Click for details

Adelante Boutique
4.0
(99)
Click for details

Balm & Bubble: Medspa | Wellness
4.8
(74)
Click for details

Benjamin Amis, MD
5.0
(257)
Click for details
The hit list

Plan your trip with Wanderboat
Welcome to Wanderboat AI, your AI search for local Eats and Fun, designed to help you explore your city and the world with ease.
Powered by Wanderboat AI trip planner.