Rush University Graduate College things to do, attractions, restaurants, events info and trip planning
Basic Info
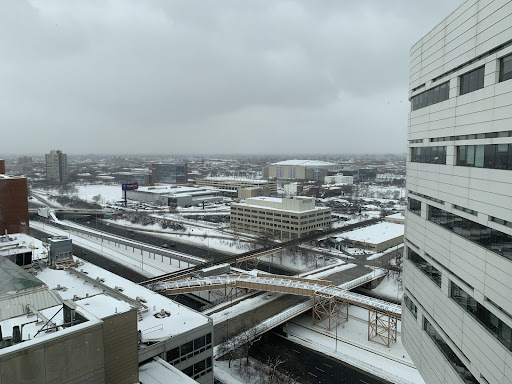
Rush University Graduate College
600 S Paulina St Suite 438, Chicago, IL 60612
4.5(171)
Open until 12:00 AM
Save
spot
spot
Ratings & Description
Info
attractions: Rush University, Cook County Hospital, University Of Illinois Dermatology, United Center, United Center, UIC School of Public Health, Michael Jordan Statue, Arrigo (Victor) Park, Skinner (Mark) Park, National Public Housing Museum, restaurants: Zenblen, Starbucks, Ms. B's Kitchen & Catering, Park Tavern, Sbarro, Panera Bread, Panera Bread, Room 500, Pompei Restaurant, Sbarro, local businesses: Rush University Medical Center, Rush University Medical College, Rush Fitness Center, Library of the Health Sciences-Chicago, University of Illinois at Chicago, UI Health, Scio at the Medical District, University of Illinois College of Medicine at Chicago, Illinois Medical District, Malcolm X College, Guest House
 Learn more insights from Wanderboat AI.
Learn more insights from Wanderboat AI.Phone
(312) 942-3589
Website
rushu.rush.edu
Open hoursSee all hours
SatClosedOpen
Plan your stay

Pet-friendly Hotels in West Chicago Township
Find a cozy hotel nearby and make it a full experience.

Affordable Hotels in West Chicago Township
Find a cozy hotel nearby and make it a full experience.

The Coolest Hotels You Haven't Heard Of (Yet)
Find a cozy hotel nearby and make it a full experience.

Trending Stays Worth the Hype in West Chicago Township
Find a cozy hotel nearby and make it a full experience.
Reviews
Live events

Chicago Underground Pedway & Secret Interiors Tour
Sat, Feb 7 • 2:00 PM
Chicago, Illinois, 60602
View details

ILAPT 2026 Annual Conference
Fri, Feb 6 • 8:30 AM
1110 Pleasant Street Oak Park, IL 60302
View details

Opening Keynote: Teresa Montoya’s Tó Łitso (Yellow Water)
Sat, Feb 7 • 2:00 PM
40 Arts Circle Drive Evanston, IL 60208
View details
Nearby attractions of Rush University Graduate College
Rush University
Cook County Hospital
University Of Illinois Dermatology
United Center
United Center
UIC School of Public Health
Michael Jordan Statue
Arrigo (Victor) Park
Skinner (Mark) Park
National Public Housing Museum

Rush University
4.4
(9)
Open 24 hours
Click for details

Cook County Hospital
4.4
(78)
Open until 12:00 AM
Click for details

University Of Illinois Dermatology
2.8
(10)
Open until 8:00 PM
Click for details
United Center
4.7
(8.9K)
Open 24 hours
Click for details
Nearby restaurants of Rush University Graduate College
Zenblen
Starbucks
Ms. B's Kitchen & Catering
Park Tavern
Sbarro
Panera Bread
Panera Bread
Room 500
Pompei Restaurant
Sbarro

Zenblen
4.7
(18)
$
Open until 12:00 AM
Click for details

Starbucks
3.6
(56)
$
Open until 9:00 PM
Click for details

Ms. B's Kitchen & Catering
4.3
(16)
Open until 12:00 AM
Click for details

Park Tavern
4.2
(687)
$$
Open until 12:00 AM
Click for details
Nearby local services of Rush University Graduate College
Rush University Medical Center
Rush University Medical College
Rush Fitness Center
Library of the Health Sciences-Chicago, University of Illinois at Chicago
UI Health
Scio at the Medical District
University of Illinois College of Medicine at Chicago
Illinois Medical District
Malcolm X College
Guest House

Rush University Medical Center
3.4
(579)
Click for details

Rush University Medical College
4.8
(16)
Click for details

Rush Fitness Center
4.4
(34)
Click for details

Library of the Health Sciences-Chicago, University of Illinois at Chicago
4.2
(48)
Click for details